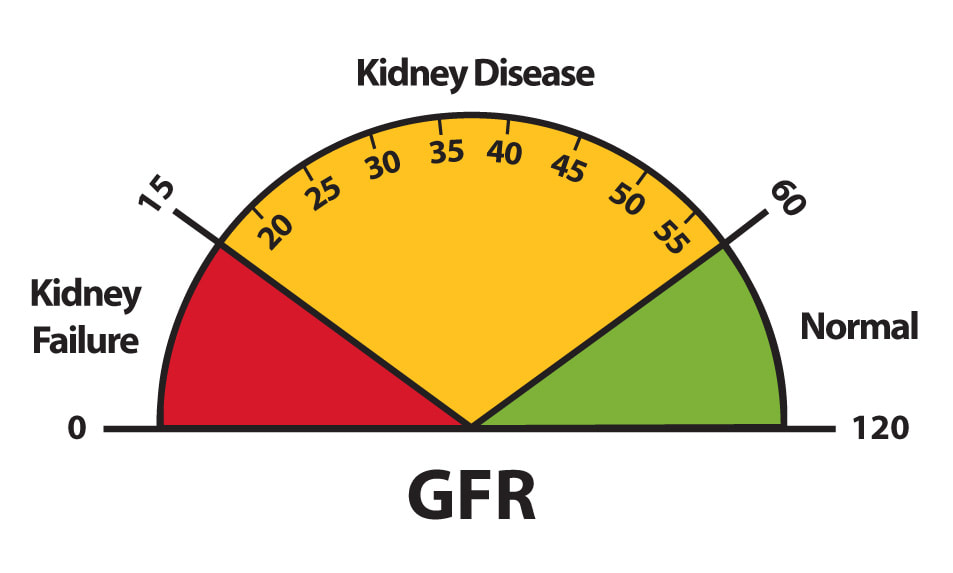
 When patients in her support group complained that they did not find out about the level/stage of their kidney function or the GFR (glomerular filtration rate) until it was too late and they were headed towards dialysis, Lana Schmidt decided to do something about it. "Blood labs throughout the United States need to change their GFR lab reporting to show the exact number of the GFR and the stage of kidney disease," says Schmidt. Currently, it is common practice to report on the blood labs GFR greater than 60 normal, when 59 is stage 3. This change is needed. "So both patients and their doctors are informed whether or not they have kidney disease and at what level." It has taken years of advocating, but Lana was able to get this change made at her local hospital in Quincy, Illinois. What difference does this make? By finding out about their GFR before a patient is considered in kidney failure, they can change their diet to slow or stop the progression, get educated about the disease, or even join one of the many programs available to learn more about it. "Finding out earlier, as we know with any disease, is always better than later," says Schmidt. Though she is happy to see the change at her local hospital, Schmidt doesn't plan on stopping to advocate for this change at other health systems nationwide.
0 Comments
Our Patient Co-Investigator, Lana Schmidt, won a KidneyX Patient Innovator Prize, funded by the National Kidney Foundation. Her project is entitled "Getting a care partner for home dialysis."
Getting a care partner for home dialysis Motivating patients to make the transition from in-center dialysis to home dialysis can be very challenging because it is an unknown and they are fearful. One way to help ease their fear is to have someone there to help them after they have gone through the training. Most states have some type of home health care program for chronically ill patients that provides the assistance they need in doing home dialysis. This type of assistance program can take the heavy burden off the patients of doing dialysis at home.  Our Patient Co-Investigator on our study, Peter Woods, who suffers from 9/11-related lung, heart, and kidney ailments, fears COVID-19 would be "a death sentence". He was recently featured in a story about this in The City, an independent, nonprofit news outlet in New York. Click here to view the full story  Our Patient Co-Investigor on our study, Patty Danielson, has been on dialysis for more than 12 years. Most patients undergo dialysis three days a week for four hours at a time, which is risky during this time of the Coronavirus. View Patty's full story on The Washington Post website here.  End-stage renal disease (ESRD) occurs when chronic kidney disease reaches an advanced state. Early in chronic kidney disease, you may have no signs or symptoms. As chronic kidney disease progresses to end-stage renal disease, signs and symptoms might include:
When should I see a doctor? Make an appointment with your doctor if you have any signs or symptoms of kidney disease. If you have a medical condition that increases your risk of kidney disease, your doctor is likely to monitor your blood pressure and kidney function with urine and blood tests during regular office visits. Ask your doctor whether these tests are necessary for you. Post submitted by Suzanne Ruff, a Patient Co-Investigator on our study.  Over 70 years ago, my mother stood next to her mother on her deathbed. My mother was a teenager at the time. My grandmother’s kidneys had failed and there was nothing the doctors could do for her. There was no dialysis, no transplants, no magic pill to save my grandmother. Over 50 years ago, my mother stood next to her sister on her deathbed. Her kidneys had failed, too. Dialysis was new and exciting, but there were not enough dialysis machines for everyone who needed one. My aunt gave up her place on the waiting list for a dialysis machine so someone else with a family could live. My aunt was a Roman Catholic nun and felt God wanted her to do that. She died at age 45. Two years later, my mom’s two brothers had kidneys that were failing. That’s when the family learned a genetic disease called polycystic kidney disease (PKD) caused all the heartache. My mother and father decided to find out (with the antiquated genetic testing of 50 years ago) whether mom and their three children had the disease. The results almost destroyed my father. Three out of four of us tested had inherited polycystic kidney disease. A disease without a cure. Dad stumbled into the gloom of depression. Alcohol was his solace. When Mom’s kidneys began to fail and she started dialysis, she often said how blessed and lucky she was because Medicare covered her dialysis. Dad was still a problem, though, and mom gave him an ultimatum: I need you. Do you know what Dad did? He stepped up, sobered up, and stood up to kidney disease with the kind of courage Dad said was given ‘by the grace of God’. He dedicated his life to being Mom’s caregiver and he did it with amazing grace. His compassion was genuine as he learned to cook and make the house sparkle. He tirelessly worked to educate himself about kidney disease, find a cure and fundraise. He wrote letters to Congress, knew his legislatures, and went to Capitol Hill. His claim to fame is that he made a telephone call that resulted in the first federal funding for research on polycystic kidney disease. Explaining why he stepped up, “It’s better than having a pity-party if you get involved.” Two months ago, I stood next to my Dad on his deathbed. Despite my tears, at 95 years of age, it was his time. I am blessed ‘by the grace of God’ to have had such a wonderful man for my father. Improving Access to Kidney Transplantation: Business as Usual or New Ways of Doing Business?9/10/2019  PREPARE NOW Principal Investigator, L. Ebony Boulware, MD, was the lead author on an Editorial published today in the Journal of American Medical Association (JAMA). The publication states: "Kidney transplantation saves lives, improves patients’ quality of life, and it is less costly in the long run compared with dialysis treatments. Despite this, kidney transplantation remains underused in the United States. Fewer than 15% of patients who initiate hemodialysis are placed on the deceased donor kidney transplantation waiting list or receive a kidney transplant within 1 year of dialysis initiation." Read the full article on the JAMA website here! Let us know in the comments below ways that you think can improve the kidney transplantation process.  This post was submitted by Hanna, a 29 year old Medical Assistant that lives in Ohio. This is her live kidney donation story. In October 2018, my co-worker's son, Brandon, came to the doctor's office not feeling well. He thought he just had a nasty cold and complained of fatigue. I was his medical assistant coincidentally that day, so the doctor saw him and ordered bloodwork that I had to draw on him. Later that day we got the test results back and I informed my coworker that he needed to take his son to the ER as soon as possible. He was in stage 5 kidney failure at the young age of 20! Everything happened so fast. They started him on dialysis immediately and he was in the hospital for a week. They finally sent him home and set him up with at-home dialysis as he was put on a waiting list for a cadaver kidney. My coworker eventually returned to work a week later. I remember talking to him in the break room asking him how his son was doing and if they knew when people could start getting tested to see if they are matches. He said that information would be coming soon. I smiled at him as I wrote my number on a post-it note and said call me when you get the information. He’s going to be okay, I’m going to be his match. My coworker, Don, had a tear running down the left cheek, I had a tear running down my right cheek. We hugged and I walked away. A few weeks passed and Don finally received the information for testing. I called and set up my appointment immediately. The end of January I had my testing. Early February I got the call stating that I was a perfect match for Brandon! I was ecstatic, but I knew I would be his match in my heart. The nurse told me that we had the same blood type and that our tissues and antibodies reacted negatively, so there was less of a chance for rejection.... AMAZING! The next step was going through an extensive head to toe physical to make sure I was healthy enough for surgery. A few weeks later, I found out that I was cleared for surgery and scheduled for my pre-op testing, more blood-work and meeting with a few people. The only way I can describe this whole experience is that GOD put this on my heart and lead me to this opportunity. My faith has brought me to giving this young man a second chance at life! Brandon and I will forever share a bond and I am blessed beyond words to share a part of myself with such an amazing young man! Before his diagnosis he was working two jobs, going to school full time, saving for a car, and enjoyed roller coasters! My wish is for him to return to all of the things he loves and is passionate about. We will get through this together. Kidney buddies for life! Hanna and Brandon underwent a successful live kidney donation surgery on June 19, 2019.  Meet Lana, a Patient Co-Investigator on our study. Learn about her and her struggles with kidney care in the spotlight below. I am passionate about raising kidney awareness throughout our nation and want to improve the quality of care and services for kidney patients, making a difference in their quality of life. I have had my own marketing consulting business for years and I use those skills to promote kidney awareness in my local community and nationwide. I was on dialysis for 13.5 years before receiving a kidney transplant using an experimental drug, which suppressed my high antibodies. I have been on all the modalities and did home hemodialysis on my own, putting in my own needles, 7 days/week for 2 hours each treatment. I have been a national patient advocate for many years and strongly believe that kidney patients talking to kidney patients is very important to improve their quality of life. Also, I want to be involved in empowering and equipping kidney patients to be fully educated in making medical decisions for their life. It is very important that kidney patients receive information about their disease and possible options as early on as possible. Why is this project important? I want to bring positive change for kidney patients, helping them to be more informed and knowledgeable about the disease and how to make the best decisions for themselves.  With kidney failure, there are three treatment options to help filter your blood and take over part of the work your damaged kidneys can no longer do. Those options are:
Living with kidney failure can be a huge challenge. It works best if you stick to your treatment schedule, review your medicines with your health care provider at every visit, follow a special eating plan, and are active most days of the week. |
Archives
September 2020
Categories |
 RSS Feed
RSS Feed
